Benefits of a modified local precision liver resection using intraoperative laparoscopic ultrasound in the treatment and prognosis of patients with liver cancer.
Beneficios de la resección hepática de precisión local modificada, utilizando ecografía intraoperatoria laparoscópica en el tratamiento y pronóstico de pacientes con cáncer de hígado.
Resumen
La tasa de incidencia y mortalidad del cáncer de hígado ha aumentado drásticamente. Además de la resección hepática abierta como método de tratamiento más común, la ecografía laparoscópica intraoperatoria (LUS) se ha utilizado recientemente en la hepatectomía. El objetivo de la investigación actual es responder a esta pregunta. 76 pacientes con cáncer de hígado ingresados en el Hospital de la Universidad de Beihua entre febrero de 2018 y septiembre de 2021 fueron asignados aleatoriamente a dos grupos de 38 pacientes, un grupo sometido a cirugía laparoscópica convencional (grupo control) y el otro grupo sometido a resección hepática laparoscópica precisa, después de colocar un instrumento LUS intraoperatorio (grupo de estudio). La pérdida de sangre y el daño a las venas hepáticas durante la cirugía fueron menores en el grupo de estudio (p < 0,05). Siete días después de la cirugía, los índices de función hepática (albúmina, bilirrubina total y alanina y aspartato aminotransferasas) e índices relacionados con la función inmune, interleucina 6, factor de necrosis tumoral α, linfocitos T CD3+ y CD4+ y nivel de células NK en el grupo de estudio mejoraron en comparación con el grupo control. Las complicaciones post- operatorias fueron menores en el grupo de estudio, y el seguimiento a los 9 meses mostró que la tasa de recurrencia fue menor y la tasa de supervivencia fue mayor en este grupo. Este estudio demuestra que la hepatectomía laparoscópica precisa modificada con el uso de la ecografía laparoscópica intraoperatoria da como resultado mejores resultados intraoperatorios y postoperatorios para el pronóstico y la tasa de supervivencia de los pacientes con cáncer de hígado, y hace que valga la pena generalizar esta técnica quirúrgica en la práctica clínica.
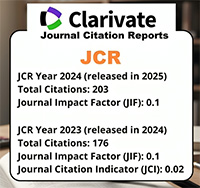
Descargas
Citas
Sun H C, Zhou J, Wang Z, Liu X, Xie Q, Jia W, Zhao M, Bi X, Li G, Bai X, Ji Y, Xu L, Zhu X D, Bai D, Chen Y, Chen Y, Dai Ch, Guo R, Guo W, Hao Ch, Huang T, Huang Zh, Li D, Li Gang, Li Tao, Li X, Li G, Liang X, Liu J, Liu F, Lu Sh, Lu Zh, Lv W, Mao Y, Shao G, Shi Y, Song T, Tan G, Tang Y, Tao K, Wan Ch, Wang G, Wang L, Wang Sh, Wen T, Xing B, Xiang B, Yan Sh, Yang D, Yin G, Yin T, Yin Zh, Yu Zh, Zhang B, Zhang J, Zhang Sh, Zhang T, Zhang Y, Zhang Y, Zhang A, Zhao H, Zhou L, Zhang W, Zhu Zh, Qin Sh, Shen F, Cai X, Teng G, Cai J, Chen M, Li Q, Liu L, Wang W, Liang T, Dong J, Chen X, Wang X, Zheng Sh, Fan J. Chinese expert consensus on conversion therapy for hepatocellular carcinoma. Hepatobiliary Surge Nutr 2021; 11(2): 227–252. https://doi. org/10.21037/hbsn-21-328.
Sasaki K, Ruffolo LI, Kim MH, Fujili M, Hashimoto K, Imaoka Y, Melcher M L, MD, Aucejo F N, Tomiyama K, Hernandez-Alejandro R. The current state of liver transplantation for colorectal liver metastases in the United States: A call for standardized reporting. Ann Surg Oncol 2023; 30: 2769–2777. https://doi.org/10.1245/ s10434-023-13147-6
.
Sena G, Paglione D, Gallo G, Goglia M, Osso M, Nardo B. Surgical resection of a recurrent hepatocellular carcinoma with portal vein thrombosis: is it a good treatment option? A case report and systematic review of the literature. J Clin Med 2022; 11(18):5287.
Shannon AH, Ruff SM, Pawlik TM. Expert insights on current treatments for hepato-cellular carcinoma: clinical and molecular approaches and bottlenecks to progress. J Hepatocell Carcinoma 2022; 9:1247-1261. https://doi.org/10.2147/JHC.S383922.
Boudjema K, Locher C, Sabbagh C, Ortega-Deballon P, Heyd B, Bachellier P, Metairie S, Paye F, Bourlier P, Adam R, Merdrignac A, Tual Ch, Pabic E L, Sulpice L, Meunier B, Regimbeau J-M, Bellissant E. Simultaneous versus delayed resection for initially resectable synchronous colorectal cancer liver metastases: A prospective, open-label, randomized, controlled trial. Ann Surg 2021;273(1):49-56. https://doi. org/10.1097/SLA.0000000000003848.
Aliseda D, Martí-Cruchaga P, Zozaya G, Rodríguez-Fraile M, Bilbao JI, Benito- Boillos A, De La Cuesta AM, Lopez- Olaondo L, Hidalgo F, Ponz-Sarvisé M, Chopitea A, Rodríguez J, Iñarrairaegui M, Herrero J I, Pardo F, Sangro B, Rotellar F. Liver resection and transplantation following Yttrium-90 radioembolization for primary malignant liver tumors: A 15- year single-center experience. Cancers 2023;15(3):733. https://doi.org/10.3390/ cancers15030733.
Naidu CS, Sarin A. Postoperative liver failure. GI Surgery Annual 2017;23:59-81.
Hou H, Zhou D, Cui X, Wang L, Wu C, Xiong Q, Geng X. Laparoscopic liver resection ameliorates the postoperative liver function impairment for hepatocellular carcinoma patients. Surg Laparosc Endosc Percutan Tech. 2020;30(1):69-73. https://doi. org/10.1097/SLE.0000000000000749.
Kuemmerli C, Fichtinger RS, Moekotte A, Aldrighetti LA, Aroori S, Besselink MGH, D’Hondt M, Díaz-Nieto R, Edwin B, Efanov M, M. Ettorre G, Menon K V, Sheen A J, Soonawalla Z, Sutcliffe R, Troisi R I, White SA, Brandts L, van Breukelen GJP, Sijberden J, Pugh SA, Eminton Z, Primrose JN, Dam RV. Laparoscopic versus open resections in the posterosuperior liver segments within an enhanced recovery programme (ORANGE Segments): study protocol for a multicentre randomised controlled trial. Trials 2022;23(1):206. https://doi.org/10.1186/ s13063-022-06112-3.
Zhang W, Zhu W, Yang J, Xiang N, Zeng N, Hu H, Jia F, Fang Ch. Augmented reality navigation for stereoscopic laparoscopic anatomical hepatectomy of primary liver cancer: Preliminary experience. Front Oncol 2021;11:663236. https://doi. org/10.3389/fonc.2021.663236.
Lam J, Tam MS, Retting RL, McLemore EC. Robotic versus laparoscopic surgery for rectal cancer: A comprehensive review of oncological outcomes. Perm J 2021;25. https://doi.org/10.7812/TPP/21.050.
Serednicki W, Hołówko W, Major P, Małczak P, Pędziwiatr M. Minimizing blood loss and transfusion rate in laparoscopic liver surgery: a review. Videosurgery and other miniinvasive techniques 2023;18(2):213-223. https://doi.org/10.5114/wiitm.2022.124088.
Qin S. Guidelines on the diagnosis and treatment of primary liver cancer (2011 edition). Chin Clin Oncol 2012;1(1):10. https://doi.org/10.3978/j.issn.2304-38 65.2012.07.01.
Huang Q, Zou MH, Jiang Y, Chen ZP, Wang Q, Wei JC, Li WL, Cao J. Outcomes of laparoscopic surgery for mucinous colorectal adenocarcinoma. J Laparoendosc Adv Surg Tech A 2021;31(6):638-647. https:// doi.org/10.1089/lap.2020.0588.
Zhou J, Sun H-C, Wang Z, Cong W-M, Wang J-H, Zeng M-S, Yang J-M, Bie P, Liu L-X, Wen T-F, Han G-H, Wang M-Q, Liu R-B, Lu L-G, Ren Zh-G, Chen M-S, Zeng Z-Ch, Liang P, Liang Ch-H, Chen M, Yan F-H, Wang W-P, Ji Y, Cheng W-W, Dai C-L, Jia W-D, Li Y-M, Li Y-X, Liang J, Liu T-Sh, Lv G-Y, Mao Y-L, Ren W-X, Shi H-Ch, Wang W-T, Wang X-Y, Xing B-C, Xu J-M, Yang J-Y, Yang Y-F, Ye Sh-L, Yin Z-Y, Zhang B-H, Zhang Sh-J, Zhou W-P, Zhu J-Y, Liu R, Shi Y-H, Xiao Y-Sh, Dai Z, Teng G-J, Cai J-Q, Wang W-L, Dong J-H, Li Q, Shen F, Qin S-K, Fanl J. Guidelines for diagnosis and treatment of primary liver cancer in China (2017 Edition). Liver Cancer 2018;7(3):235-260. https://doi. org/10.1159/000488035.
Liu Y, Wang Q, Du B, Wang XZ, Xue Q, Gao WF. Meta-analysis of indocyanine green fluorescence imaging-guided laparoscopic hepatectomy. Photodiagnosis Photodyn Ther 2021;35:102354. https:// doi.org/10.1016/j.pdpdt.2021.102354.18.
Ibuki S, Hibi T, Tanabe M, Geller DA, Cherqui D, Wakabayashi G. Short-term outcomes of “difficult” laparoscopic liver resection at specialized centers: Report from INSTALL (International Survey on Technical Aspects of Laparoscopic Liver Resection)-2 on 4478 patients. Ann Surg 2022;275(5):940-946. https://doi. org/10.1097/SLA.0000000000004434.
Matsukuma S, Tokumitsu Y, Nakagami Y, Shindo Y, Matsui H, Nakajima M, Iida M, Suzuki N, Takeda Sh, Nagano H. Laparoscopic resection reduces superficial surgical site infection in liver surgery. Surg Endosc 2021;35(12):7131-7141. https:// doi.org/10.1007/s00464-020-08233-9.
Huang Y, Chen F, Li H. Effect of rapid rehabilitation nursing on inflammation and liver function after laparoscopic radical resection of primary liver cancer. Am J Transl Res 2022;14(11):8156-8165.
Fu XT, Tang Z, Chen JF, Shi YH, Liu WR, Gao Q, Ding G-Y, Song K, Wang X-Y, Zhou J, Fan J, Ding Z-B. Laparoscopic hepatectomy enhances recovery for small hepatocellular carcinoma with liver cirrhosis by postoperative inflammatory response attenuation: a propensity score matching analysis with a conventional open approach. Surg Endosc 2021;35(2):910-920. https://doi. org/10.1007/s00464-020-07710-5.
Schag CC, Heinrich RL, Ganz PA. Karnofsky performance status revisited: reliability, validity, and guidelines. J Clin Oncol 1984;2(3):187-193. https://doi. org/10.1200/JCO.1984.2.3.187.
Allaire M, Goumard C, Lim C, Le Cleach A, Wagner M, Scatton O. New frontiers in liver resection for hepatocellular carcinoma. JHEP Rep 2020;2(4):100134. https:// doi.org/10.1016/j.jhepr.2020.100134.
Sugawara Y, Hibi T. Surgical treatment of hepatocellular carcinoma. BioSci Trends 2021;15(3):138-41. https://doi. org/10.5582/bst.2021.01094.
Lubner MG, Mankowski Gettle L, Kim DH, Ziemlewicz TJ, Dahiya N, Pickhardt P. Diagnostic and procedural intraoperative ultrasound: technique, tips and tricks for optimizing results. Br J Radiol 2021;94(1121):20201406. https://doi.org/10.1259/bjr.20201406.
Joliat G-R, Kobayashi K, Hasegawa K, Thomson J-E, Padbury R, Scott M, Brustia R, Scatton O, Cao HST, Vauthey J-N, Dincler S, Clavien P-A, Wigmore SJ, Demartines N, Melloul E. Guidelines for perioperative care for liver surgery: Enhanced Recovery After Surgery (ERAS) Society Recommendations 2022. World J Sur 2023;47(1):11-34. https://doi.org/10. 1259/bjr.20201406.
Tayar DO, Ribeiro U, Jr., Cecconello I, Magalhães TM, Simões CM, Auler JOC, Jr. Propensity score matching comparison of laparoscopic versus open surgery for rectal cancer in a middle-income country: short-term outcomes and cost analysis. Clinicoecon Outcomes Res 2018;10:521-527. https://doi.org/10.2147/CEOR.S173718.
Morise Z, Katsuno H, Kikuchi K, Endo T, Matsuo K, Asano Y, Horiguchi A. Laparoscopic repeat liver resection-selecting the best approach for repeat liver resection. Cancers 2023;15(2):421. https://doi. org/10.3390/cancers15020421.
Berardi G, Muttillo EM, Colasanti M, Mariano G, Meniconi RL, Ferretti S, Guglielmo N, Angrisani M, Lucarini A, Garofalo E, Chiappori D, Di Cesare L, Vallati D, Mercantini P, Ettorre GM. Challenging scenarios and debated indications for laparoscopic liver Resections for hepatocellular carcinoma. Cancers 2023;15(5):1493. https://doi.org/ 10.3390/cancers15051493.
Dąbrowska AM, Słotwiński R. The immune response to surgery and infection. Cent Eur J Immunol 2014;39(4):532-537. https://doi.org/10.5114/ceji.2014.47741.
Amodeo G, Bugada D, Franchi S, Moschetti G, Grimaldi S, Panerai A, Allegri M, Sacerdote P. Immune function after major surgical interventions: the effect of postoperative pain treatment. J Pain Res 2018;11:1297-1305. https://doi.org/ 10.2147/JPR.S158230.
Elshazly M, Khair T, Bassem M, Mansour M. The use of intraoperative bedside lung ultrasound in optimizing positive end expiratory pressure in obese patients undergoing laparoscopic bariatric surgeries. Surg Obes Relat Dis 2021;17(2):372-378. https://doi. org/10.1016/j.soard.2020.09.023.
Kurilova I, Bendet A, Petre EN, Boas FE, Kaye E, Gonen M, Covey A, Brody LA, Brown KT, Kemeny NE, Yarmohammadi H, Ziv E, D’Angelica MI, Kingham TP, Cercek A, Solomon SB, Beets-Tan RGH, Sofocleous CT. Factors associated with local tumor control and complications after thermal ablation of colorectal cancer liver metastases: a 15-year retrospective cohort study. Clinical Colorectal Cancer 2021;20(2):e82-e95. https://doi. org/10.1016/j.clcc.2020.09.005.
Skrzep-Poloczek B, Poloczek J, Chełmecka E, Kazura W, Dulska A, Idzik M, Jochem J, Stygar D. General, 21-day postoperative rehabilitation program has beneficial effect on oxidative stress markers in patients after total hip or knee replacement. Oxid Med Cell Longev 2020; 2020:4598437. https://doi. org/10.1155/2020/4598437.