Effect of anesthetic, analgesic and sedative agents on human cell phagocytosis. Review. /
Resumen
Abstract.
Along with preoperative stress, anesthetics per se are associated with decreased activity of the immune system. Phagocytosis is an important process where particles, such as dead cells and bacteria, are eliminated from the organism. This process is complex and involves cell chemotaxis, tissue infiltration, several coordinated cellular events and the production of reactive oxygen and nitrogen species (ROS). Therefore, the aim of this review was to report the effects of anesthetic, analgesic and sedative agents on human cell phagocytosis. This review suggests that human phagocytosis processes are affected by main anesthetic, analgesic and sedatives agents that result in decreased chemotaxis, phagocytosis and ROS production. These effects may impair the anti-bacterial function of phagocytes. Clinical anesthesiologists should select the anesthetics and the anesthetic methods with careful consideration of the clinical situation and the immune status of patients, concerning long-term mortality, morbidity, and the optimal prognosis.
Resumen.
La anestesia y el estrés preoperatorio están asociados a la depresión del sistema inmunitario. La fagocitosis es un proceso importante destinado a la eliminación de células muerta y microorganismos. Es un proceso complejo que involucra la quimiotaxis celular, la infiltración tisular leucocitaria y la activación de diversos procesos intracelulares coordinados, que incluyen la producción de especies reactivas de oxígeno y nitrógeno (ERON). Por lo tanto, el propósito de esta revisión fue reportar el efecto de agentes anestésicos, analgésicos y sedativos en la fagocitosis humana. Esta revisión sugiere que los procesos relacionados con la fagocitosis humana son afectados por los principales agentes anestésicos, analgésicos y sedativos, que inducen una disminución de la quimiotaxis, fagocitosis y producción de ERON y la función anti-bacterial de los fagocitos. Los anestesiólogos clínicos deben seleccionar los anestésicos y los métodos de anestesia, considerando la situación clínica y el estado inmunitario de los pacientes en relación a la mortalidad, morbilidad y pronóstico óptimo a largo plazo.
Descargas
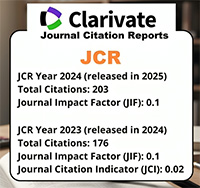
Citas
Miller RD. Miller’s Anesthesia. 7th ed. USA: Churchill Livingstone Elsevier; 2010.
Richards DM, Endres RG. How cells engulf: a review of theoretical approaches to phago- cytosis. Rep Prog Phys 2017; 80: 1-51. doi: 10.1088/1361-6633/aa8730.
Friedman H, Newton C, Klein TW. Microbial infections, immunomodulation, and drugs of abuse. Clin Microbiol Rev 2003; 16: 209–219. doi: 10.1128/cmr.16.2.209-219.2003.
Kurosawa S, Kato M. Anesthetics, immune cells, and immune responses. J Anesth 2008; 22: 263–277. doi: 10.1007/s00540-008-0626-2.
Anderson SL, Duke-Novakovski T, SinghB. The immune response to anesthesia: part 2 sedatives, opioids, and injectable an- esthetic agents. Vet Anaesth Analg 2014; 41: 553-566. doi: 10.1111/vaa.12191
Heine J, Jaeger K, Osthaus A, Weingaert- ner N, Münte S, Piepenbrock S, Leuwer M. Anaesthesia with propofol decreases FMLP- induced neutrophil respiratory burst but not phagocytosis compared with isoflurane. Br J Anaesth 2000; 85:424-430. https:// doi.org/10.1093/bja/85.3.424
Carrera JA, Catalá J, Monedero P, Hidalgo F, Carrascosa F, Arroyo JL. Comparison of the effects of isoflurane and alfentanyl on the mononuclear-phagocytic system. Rev Esp Anestesiol Reanim 1993; 40: 3-8.
Clark P, Layon AJ, Duff P. Effect of iso- flurane on neutrophil phagocytic func- tion during pregnancy. Infect Dis Obstet Gynecol 1993; 1: 98-103. doi: 10.1155/ S1064744993000237.
Du X, Jiang C, Lv Y, Dull RO, Zhao YY, Schwartz DE, Hu G. Isoflurane promotes phagocytosis of apoptotic neutrophils through AMPK-mediated ADAM17/Mer sig- naling. PLoS One 2017; 12: e0180213. doi: 10.1371/journal.pone.0180213.
Lieners C, Redl H, Schlag G, Hammer- schmidt DE. Inhibition by halothane, but not by isoflurane, of oxidative response to opsonized zymosan in whole blood. Inflam- mation 1989; 13: 621-630.
Kotani N, Hashimoto H, Sessler DI, Kiku- chi A, Suzuki A, Takahashi S, Muraoka M, Matsuki A. Intraoperative modulation of alveolar macrophage function during iso- flurane and propofolanesthesia. Anesthesi- ology 1998; 89: 1125-1132.
Koutsogiannaki S, Bernier R, Tazawa K, Yuki K. Volatile Anesthetic Attenuates Phagocyte Function and Worsens Bacterial Loads in Wounds. J Surg Res 2019; 233:323- 330. doi: 10.1016/j.jss.2018.07.075.
Ciepichał J, Kübler A. Effect of general and regional anesthesia on some neutrophil functions. Arch Immunol Ther Exp (Warsz) 1998; 46: 183-192.
Khan FA, Kamal RS, Mithani CH, Khur- shid M. Effect of general anaesthesia and surgery on neutrophil function. Anaes- thesia 1995; 50: 769-775. https://doi. org/10.1111/j.1365-2044.1995.tb06137.x
Barth J, Petermann W, Entzian P, Wustrow C, Wustrow J, Ohnhaus EE. Modulation of oxygen-free radicals from human leuko- cytes during halothane- and enflurane- in- duced general anesthesia. Acta Anaesthe- siol Scand 1987; 31:740-743. https://doi. org/10.1111/j.1399-6576.1987.tb02656.x
Nunn JF, Sturrock JE, Jones AJ, O’Moráin C, Segal AW, Coade SB, Dorling J, Walker D. Halothane does not inhibit human neu- trophil function in vitro. Br J Anaesth 1979; 51: 1101-1108.
Erol A, Reisli R, Reisli I, Kara R, Otelcio- glu S. Effects of desflurane, sevoflurane and propofol on phagocytosis and respira- tory burst activity of human polymorphonu- clear leucocytes in bronchoalveolar lavage. Eur J Anaesthesiol 2009; 26:150-154. doi: 10.1097/EJA.0b013e328319bfeb.
Fahlenkamp AV, Coburn M, Rossaint R, Stoppe C, Haase H. Comparison of the ef- fects of xenon and sevoflurane anaesthesia on leucocyte function in surgical patients: a randomized trial. Br J Anaesth 2014; 112: 272-280. doi: 10.1093/bja/aet330.
Perttilä J, Lilius EM, Salo M. Ef- fects of anaesthesia and surgery on se- rum opsonic capacity. Acta Anaesthe- siol Scand 1986; 30:173-176. https://doi. org/10.1111/j.1399-6576.1986.tb02391.x
De Rossi L, Gott K, Horn N, Hecker K, Hutschenreuter G, Rossaint R. Xenon pre- serves neutrophil and monocyte function in human whole blood. Can J Anaesth 2002; 49: 942-945. doi: 10.1007/BF03016879.
Mackenzie N, Grant IS. Propofol for intra- venous sedation. Anaesthesia 1987; 42: 3–6.
Wilson E, David A, MacKenzie N, Grant IS. Sedation during spinal anaesthesia: comparison of propofol and midazolam. Br J Anaesth 1990; 64: 48–52.
Bali M, Akabas MH. Defining the propo- fol binding site location on the GABAA receptor. Mol Pharmacol 2004; 65: 68–76. https://doi.org/10.1093/bja/64.1.48.
Ince C, Coremans JM, Ypey DL, Leijh PC, Verveen AA, van Furth R. Phagocytosis by human macrophages is accompanied by changes in ionic channel currents. J Cell Biol 1988; 106: 1873–1878. doi:10.1083/ jcb.106.6.1873.
Wheeler DW, Thompson AJ, Corletto F, Reckless J, Loke JCT, Lapaque N, Grant AJ, Mastroeni P, Grainger DJ, Padgett CL, O’Brien JA, Miller NG, Trowsdale J, Lummis SC, Menon DK, Beech JS. Anaes- thetic impairment of immune function is mediated via GABAA receptors. PLoS ONE 2011; 6: e17152. doi:10.1371/journal. pone.0017152.
Shiratsuchi H, Kouatli Y, Yu GX, Marsh HM, Basson MD. Propofol inhibits pres- sure-stimulated macrophage phagocytosis via the GABAA receptor and dysregulation of p130cas phosphorylation. Am J Physiol Cell Physiol 2009; 296: C1400-1410. doi: 10.1152/ajpcell.00345.2008.
Mikawa K, Akamatsu H, Nishina K, Shiga M, Maekawa N, Obara H, Niwa Y. Propo- fol inhibits human neutrophil functions. Anesth Analg 1998; 87: 695-700. doi: 10.1213/00000539-199809000-00039.
Heller A, Heller S, Blecken S, Urbas- chek R, Koch T. Effects of intravenous anesthetics on bacterial elimination in human blood in vitro. Acta Anaesthesiol Scand 1998; 42: 518-526. https://doi. org/10.1111/j.1399-6576.1998.tb05160.x
Krumholz W, Endrass J, Hempelmann G. Propofol inhibits phagocytosis and killing of Staphylococcus aureus and Escherichia coli by polymorphonuclear leukocytes in vitro. Can J Anaesth 1994; 41: 446-449. doi:10.1007/BF03009871.
Ploppa A, Kiefer RT, Krueger WA, Unertl KE, Durieux ME. Local anesthetics time- dependently inhibit staphylococcus aureus phagocytosis, oxidative burst and CD11b expression by human neutrophils. Reg Anesth Pain Med 2008; 33: 297-303. doi: 10.1016/j.rapm.2007.05.012.
Bravo J, Zúñiga M, Carrero Y, Mosquera J. Propofol, fentanyl and remifentanil do not impair the phagocytic capacity to Candida albicans of human peripheral blood poli- morphonuclear cells. Rev Chi Anestesiol 2019; 48: 459-462. doi:10.25237/revchilanestv48n05.11.
Corcoran TB, Engel A, Sakamoto H, O’Shea A, O’Callaghan-Enright S, Short- en GD. The effects of propofol on neu- trophil function, lipid peroxidation and inflammatory response during elective coronary artery bypass grafting in patients with impaired ventricular function. Br J An- aesth 2006; 97:825-831. doi: 10.1093/bja/ ael270.
Davidson JA, Boom SJ, Pearsall FJ, Zhang P, Ramsay G. Comparison of the effects of four i.v. anaesthetic agents on poly- morphonuclear leucocyte function. Br J Anaesth 1995; 74: 315-318. https://doi. org/10.1093/bja/74.3.315.
Huettemann E, Jung A, Vogelsang H, Hout Nv, Sakka SG. Effects of propofol vs methohexital on neutrophil function and immune status in critically ill patients. J Anesth 2006; 20: 86-91.
Skoutelis A, Lianou P, Papageorgiou E, Kokkinis K, Alexopoulos K, Bassaris H. Effects of propofol and thiopentone on polymorphonuclear leukocyte functions in vitro. Acta Anaesthesiol Scand 1994; 38: 858-862. https: //doi.org/ 10.1111/j.1399- 6576.1994.tb04018.x.
Yu G, Dymond M, Yuan L, Chaturvedi LS, Shiratsuchi H, Durairaj S, Marsh HM, Bas- son MD. Propofol’s effects on phagocytosis, proliferation, nitrate production, and cyto- kine secretion in pressure-stimulated mi- croglial cells. Surgery 2011; 150: 887-896. doi: 10.1016/j.surg.2011.04.002.
Chang Y, Chen TL, Sheu JR, Chen RM. Suppressive effects of ketamine on mac- rophage functions. Toxicol Appl Pharma- col 2005; 204: 27-35. doi:10.1016/j.taap.2004.08.011.
Krumholz W, Endrass J, Knecht J, Hemp- elmann G. The effects of midazolam droperidol, fentanyl, and alfentanil on phagocytosis and killing of bacteria by poly- morphonuclear leukocytes in vitro. Acta Anaesthesiol Scand 1995; 39: 624-627. https://doi.org/10.1111/j.1399-6576.1995. tb04138.x.
Toyota S, Moriyama M, Otake T, Kono J, Shudou Y, Satake T, Seki K, Masuda S, Amaki Y. Effect of anaesthetic agents on the phagocytic function of human poly- morphonuclear leukocytes through analysis with a phagocytic plaque method. Inflamm Res 1995; 44: 204-206.
Nishina K, Akamatsu H, Mikawa K, Shiga M, Maekawa N, Obara H, Niwa Y. The in- hibitory effects of thiopental, midazolam, and ketamine on human neutrophil func- tions. Anesth Analg 1998; 86: 159-165. doi: 10.1213/00000539-199801000-00032.
Krumholz W, Endrass J, Hempelmann G. Inhibition of phagocytosis and killing of bacteria by anaesthetic agents in vitro. Br J Anaesth 1995; 75: 66-70. https://doi. org/10.1093/bja/75.1.66.
Weiss M, Buhl R, Mirow N, Birkhahn A, Schneider M, Wernet P. Do barbiturates impair zymosan-induced granulocyte func- tion? J Crit Care 1994; 9: 83-89. https:// doi.org/10.1016/0883-9441(94)90018-3.
Ploppa A, Kiefer RT, Nohé B, Haeberle HA, Dieterich HJ, Unertl KE, Durieux ME, Krueger WA. Monocyte phagocytosis of vi- able Staphylococcus aureus is impaired by barbiturates, but not by propofol. Infection 2008; 36: 220-225. doi: 10.1007/s15010-007-7240-3.
Nishina K, Akamatsu H, Mikawa K, Shiga M, Maekawa N, Obara H, Niwa Y. The ef- fects of clonidine and dexmedetomidine on human neutrophil functions. Anesth Analg 1999; 88: 452-458. doi: 10.1213/00000539-199902000-00042.
Chen SL, Zhou W, Hua FZ, Chen Y, Zheng XL, Long XF, Lu J. In vitro effect of dex- medetomidine on the respiratory burst of neutrophils. Genet Mol Res 2016; 15: 1-9. doi: 10.4238/gmr.15028069.
Wang Q, Wei H, Fan Z, Lu Y. Effect of nor- floxacin and clonidine on human trabecular meshwork cells in vitro. Graefes Arch Clin Exp Ophthalmol 1994; 232: 566-571.
Ploppa A, Kiefer RT, Nohé B, Haeberle HA, Dieterich HJ, Unertl KE, Krueger WA. Dose- dependent influence of barbiturates but not of propofol on human leukocyte phagocyto- sisof viable Staphylococcus aureus. Crit Care Med 2006; 34: 478-483. doi:10.1097/01. CCM.0000199067.71968.6E.
Marino F, Cattaneo S, Cosentino M, Ra- sini E, Di Grazia L, Fietta AM, Lecchini S, Frigo G. Diazepam stimulates migration and phagocytosis of human neutrophils: possible contribution of peripheral-type benzodiazepine receptors and intracellular calcium. Pharmacology. 2001; 63: 42-49. doi: 10.1159/000056111.
Covelli V, Munno I, Decandia P, Altamura M, Cannuscio B, Maffione AB, Jirillo E. Effects of benzodiazepines on the immune system. Acta Neurol (Napoli) 1991; 13: 418-423.
Covelli V, Maffione AB, Greco B, Can- nuscio B, Calvello R, Jirillo E. In vivo effects of alprazolam and lorazepam on the immune response in patients with migraine without aura. Immunopharma- col Immunotoxicol 1993; 15: 415-428. doi:10.3109/08923979309035237.
Traykov T, Hadjimitova V, Goliysky P, Rib- arov S. Effect of phenothiazines on activat- ed macrophage-induced luminol-dependent chemiluminescence. Gen Physiol Biophys 1997; 16: 3-14.
Trush MA, Van Dyke K. Effect of prometha- zine on human polymorphonuclear che- miluminescence. Pharmacology 1978;16:314-320. doi:10.1159/000136787.
DeChatelet LR, Qualliotine-Mann D, Caldwell R, McCall CE, Gusdon JP. Effects of promethazine-hydrochloride on human polymorphonuclear leukocytes. Infect Im- mun 1973; 7: 403-408.
Ordway D, Viveiros M, Leandro C, Jorge Arroz M, Molnar J, Kristiansen JE, Amaral L. Chlorpromazine has intracellular killing activity against phagocytosed Staphylococ- cus aureus at clinical concentrations. J Infect Chemother 2002; 8: 227-231. doi: 10.1007/s10156-002-0188-4.
Menzebach A, Hirsch J, Nöst R, Mogk M, Hempelmann G, Welters ID. Morphine in- hibits complement receptor expression, phagocytosis and oxidative burst by a nitricoxide dependent mechanism. Anasthesiol Intensivmed Notfallmed Schmerzther 2004; 39: 204-211. doi: 10.1055/s-2004-814389.
Yeager MP, Procopio MA, DeLeo JA, Ar- ruda JL, Hildebrandt L, Howell AL. In- travenous fentanyl increases natural killer cell cytotoxicity and circulating CD16(+) lymphocytes in humans. Anesth Analg 2002; 94: 94-99. doi: 10.1213/00000539-200201000-00018.
Welters ID, Menzebach A, Goumon Y, Langefeld TW, Teschemacher H, Hemp- elmann G, Stefano GB. Morphine sup- presses complement receptor expression, phagocytosis, and respiratory burst in neu- trophils by a nitric oxide and mu(3) opiate receptor-dependent mechanism. J Neuro- immunol 2000; 111:139-145. https://doi. org/10.1016/S0165-5728(00)00401-x.
Perttilä J, Lehtonen OP, Salo M, Tertti R. Effects of coronary bypass surgery un- der high-dose fentanyl anaesthesia on granulocyte chemiluminescence. Br J An- aesth 1986; 58:1027-1030. https://doi. org/10.1093/bja/58.9.1027.
Jinnouchi A, Aida Y, Nozoe K, Maeda K, Pabst MJ. Local anesthetics inhibit priming of neutrophils by lipopolysaccharide for en- hanced release of superoxide: suppression of cytochrome b558 expression by disparate mechanisms. J Leukoc Biol 2005; 78: 1356-1365. doi:10.1189/jlb.0305169.
Welters ID, Menzebach A, Langefeld TW, Menzebach M, Hempelmann G. In- hibitory effects of S-(-) and R-(+) bu- pivacaine on neutrophil function. Acta Anaesthesiol Scand 2001; 45:570-575. https://doi.org/10.1034/j.1399-6576. 2001.045005570.x.
Mikawa K, Akamarsu H, Nishina K, Shiga M, Obara H, Niwa Y. Effects of ropivacaine on human neutrophil function: comparison with bupivacaine and lidocaine. Eur J An- aesthesiol 2003; 20: 104-110.
Kawasaki C, Kawasaki T, Ogata M, Sata T, Chaudry IH. Lidocaine enhances apop- tosis and suppresses mitochondrial func- tions of human neutrophil in vitro. J Trauma 2010; 68: 401-408. doi: 10.1097/ TA.0b013e3181af6e56.
Azuma Y, Ohura K. Immunological modu- lation by lidocaine-epinephrine and prilocaine-felypressin on the functions related to natural immunity in neutrophils and macrophages. Curr Drug Targets Immune Endocr Metabol Disord 2004; 4: 29-36.
Jurjus AR, Jarrush-Saadeh D, Nassar C. Modulation of some human mononuclear cells activities by procaine. Middle East J Anaesthesiol 1988; 9: 417-428.
Heine J, Jaeger K, Weingaertner N, Scheinichen D, Marx G, Piepenbrock S. Effects of different preparations of pro- pofol, diazepam, and etomidate on hu- man neutrophils in vitro. Acta Anaesthe- siol Scand 2001; 45: 213-220. https://doi. org/10.1034/j.1399-6576.2001.450213.x.
Schneemilch CE, Bank U. Release of pro- and anti-inflammatory cytokines during dif- ferent anesthesia procedures. Anaesthesiol Reanim 2001; 26: 4–10.
Sanders RD, Hussell T, Maze M. Seda- tion and immunomodulation. Crit Care Clin 2009; 25: 551–570. doi: 10.1016/j. ccc.2009.05.001.
Odunayo A, Dodam JR, Kerl ME, DeClue AE. Immunomodulatory effects of opioids. J Vet Emerg Crit Care 2010; 20: 376–385. doi: 10.1111/j.1476-4431.2010.00561.x.
Mao L, Lin S, Lin J. The effects of anes- thetics on tumor progression. Int J Physiol Pathophysiol Pharmacol 2013; 5: 1–10.
Liu S, Carpenter RL, Neal JM. Epidural an- esthesia and analgesia. Their role in postop- erative outcome. Anesthesiology 1995; 82: 1474-1506.
Tuman KJ, McCarthy RJ, March RJ, De- Laria GA, Patel RV, Ikankovich AD. Effects of epidural anesthesia and analgesia on co- agulation and outcome after mayor vascular surgery. Anesth Analg 1991; 73: 696-704.
Moding J. The role of lumbar epidural an- esthesia as antithrombotic prophylaxis and total hip replacement. Acta Chirurgical Scand 1985; 151: 589-594.
Capdevila X, Barthelet Y, Biboulet P, Ryck- waert Y, Rubenovitch J, d’Athis F. Effects of perioperative analgesic technique on the surgical outcome and duration of rehabili- tation after major knee surgery. Anesthesi- ology, 1999; 91: 8-15.
Horlocker TT, Wedel DJ. Complicaciones in- fecciosas de la anestesia regional. Best Pract Res Clin Anaesthesiol. 2008; 22 (3): 451-75.