Species identification of non-tuberculous mycobacteria // Identificación de micobacterias no tuberculosas a nivel de especie
Resumen
Abstract
Non-tuberculous mycobacteria (NTM) prevalence has risen during recent decades. NTM species identification is crucial for treatment and epidemiologic control since, as opportunistic pathogens, they become sources of infections. Classical biochemical tests and phenotypic methods are not accurate and are time consuming. Other accurate and reliable species identification methods are available. Most are DNA-based from simple PCR-based to those more complex and high-tech based. Not all laboratories can afford technology transfer from simple to more complex and expensive methods, especially in lowincome countries. The price has dropped for some high-tech methods, hence we may think about its possible widespread use, even though some limitations exist regarding data analysis and skill acquisitions. The identification of NTM has been problematic due to their evolving taxonomy, limitations of current phenotypic methods, and absence of a universal gene target for reliable speciation. Accurate NTM identification is a challenging task in diagnostic laboratories due to the absence of a universal robust method and to the difficulty to distinguish between closely related species. This work reviews the most commonly available methods for NTM species identification nowadays.
Resumen
La prevalencia de las micobacterias no tuberculosas (MNT) se ha incrementado durante las recientes décadas. La identificación de las MNT a nivel de especies es crucial tanto para el tratamiento como para el control epidemiológico, debido a que son patógenos oportunistas y se vuelven fuentes de infección. Las pruebas bioquímicas clásicas y los métodos fenotípicos no son precisos y consumen un tiempo considerable para obtener resultados. Existen métodos precisos y confiables, la mayoría moleculares, desde aquellos basados en PCR hasta otros más complejos de alta tecnología. No todos los laboratorios pueden costear una transferencia de tecnología de métodos simples a más complejos y costosos, sobre todo en países con bajos recursos. El precio ha caído para algunos métodos tecnológicamente avanzados, por lo que se pudiera pensar en su amplio uso, aunque todavía existen limitantes en relación al análisis de datos y la adquisición de destrezas. La identificación de MNT ha sido problemática debido a: una taxonomía en constante evolución, limitaciones de los métodos fenotípicos actuales y la ausencia de un marcador genético universal para una especiación confiable. La identificación precisa de MNT es una tarea desafiante en los laboratorios que hacen diagnóstico debido a la ausencia de un método robusto universal y a la dificultad de distinguir entre especies estrechamente relacionadas. Este trabajo revisa los métodos más comunes disponibles para la identificación de las especies de MNT hasta el presente.
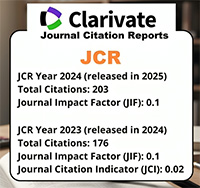
Descargas
Citas
Gunaratnam PJ, Britton WJ, Hofmeyr A. Bug breakfast in the bulletin: leprosy. N S W Public Health Bull 2013; 24: 50.
WHO.World health organization global tuberculosis report. Geneva. WHO 2014; 1-170.
Sequera M, Delgado V, Araque W, Torrealba M, Núñez R, Da Mata O, Abadía E, Takiff H, de Waard J. Mycobacterium tuberculosis:spoligotypes in the Carabobo state, Venezuela. Rev Chil Infectologia 2008; 25: 362–367.
Abadía E, Sequera M, Ortega D, Méndez MV, Escalona A, Da Mata O, Izarra E, Rojas Y, Jaspe R, Motiwala A, Alland D, de Waard J, Takiff H. Mycobacterium tuberculosis ecology in Venezuela: epidemiologic correlates of common spoligotypes and a large clonal cluster defined by MIRU-VNTR-24. BMC Infect Dis 2009; 9: 122-133.
Zhang J, Abadia E, Refregier G, Tafaj S, Boschiroli M, Guillard B, Andremont A, Ruimy R, Sola C. Mycobacterium tuberculosis complex CRISPR genotyping: improving efficiency, throughput and discriminative power of “spoligotyping” with new spacers and a microbead-based hybridization assay. J Med Microbiol 2010; 59: 285–294.
Abadia E, Zhang J, dos Vultos T, Ritacco V, Kremer K, Aktas E, Matsumoto T, Refregier G, van Soolingen D, Gicquel B, Sola C. Resolving lineage assignation on Mycobacterium tuberculosis clinical isolates classified by spoligotyping with a new highthroughput 3R SNPs based method. Infect Genet Evol 2010; 10: 1066–1074.
Abadia E, Zhang J, Ritacco V, Kremer K, Ruimy R, Rigouts L, Gomes H, Elias A, Fauville-Dufaux M, Stoffels K, Rasolofo-Razanamparany V, Garcia de Viedma D, Herranz M, Al-Hajoj S, Rastogi N, Garzelli C, Tortoli E, Suffys PN, van Soolingen D, Refrégier G, Sola C.The use of microbeadbased spoligotyping for Mycobacterium tuberculosiscomplex to evaluate the quality of the conventional method: providing guidelines for quality qssurance when working on membranes. BMC Infect Dis 2011; 11: 110-117.
Bergval I, Sengstake S, Brankova N, Levterova V, Abadía E, Akhalaia M, Tuin K, Schuitema A, Panaiatov S, Bachiyska E, Herrewegh A, Schürch A, van Soolingen D, van ‘t Hoog A, Cobelens F, Aspindzelashvili R, Sola C, Klatser P, Anthony R. Combined species identification, genotyping, and drug resistance detection of Mycobacterium tuberculosiscultures by MLPA on a bead-based array. Plos One 2012; 7: e43240. 1- 16.
Gomgnimbou M, Abadia E, Zhang J, Refrégier G, Panaiotov S, Bachiyska S, Sola C. “Spoligoriftyping,” a dual-priming-oligonucleotide-based direct-hybridization assay for tuberculosis control with a multianalyte microbead-based hybridization system. J Clin Microbiol 2012; 50: 3172–3179.
Sengstake S, Bablishvili N, Schuitema A, Bzekalava N, Abadia E, de Beer J, Tadumadze N, Akhalaia M, Tuin K, Tukvadze N, Aspindzelashvili R, Bachiyska E, Panaiotov S, Sola C, van Soolingen D, Klatser P, Anthony R, Bergval I. Optimizing multiplex SNP-based data analysis for genotyping of Mycobacterium tuberculosisisolates. BMC Genomics 2014; 15: 572-582.
Patiño M, Abadía E, Gómez S, Maes M, Muñoz M, Gómez D, Guzmán P, Méndes M, Ramirez C, España M, de Waard J, Takiff H. Mycobacterium tuberculosispopulation structure and molecular epidemiological analysis in Sucre municipality, Miranda state, Venezuela. Invest Clin 2014; 55: 332–351.
Refrégier G, Abadia E, Matsumoto T, Ano H, Takashima T, Tsuyuguchi I, Aktas E, Cömert F, Gomgnimbou M, Panaiotov S, Phelan J, Coll F, McNerney R, Pain A, Clark T, Sola C.Turkish and Japanese Mycobacterium tuberculosis sublineages share a remote common ancestor. Infect Genet Evol 2016; 45: 461–473.
Cook J. Nontuberculous mycobacteria: opportunistic environmental pathogens for predisposed hosts. Br Med Bull 2010; 96: 45–59.
Jagielski T, Minias A, van Ingen J, Rastogi N, Brzostek A, Żaczek A, Dziadek J. Methodological and clinical aspects of the molecular epidemiology of Mycobacterium tuberculosisand other mycobacteria. Clin Microbiol Rev 2016; 29: 239–290.
Timpe A, Runyon E. The relationship of atypical acid-fast bacteria to human disease; a preliminary report. J Lab Clin Med 1954; 44: 202–209.
Rindi L, Garzelli C. Increase in non-tuberculous mycobacteria isolated from humans in Tuscany, Italy, from 2004 to 2014. BMC Infect Dis 2015; 16: 44-48.
Tortoli E. Clinical manifestations of nontuberculous mycobacteria infections. Clin Microbiol Infect 2009; 15: 906–910.
Lai C, Tan C, Chou C, Hsu H, Liao C, Huang Y, Yang P, Luh K, Hsueh P. Increasing incidence of nontuberculous mycobacteria, Taiwan, 2000-2008. Emerg Infect Dis 2010; 16: 294–296.
Marras T, Daley C. Epidemiology of human pulmonary infection with nontuberculous mycobacteria. Clin Chest Med 2002; 23: 553–567.
Johnson M, Odell J. Nontuberculous mycobacterial pulmonary infections. J Thorac Dis 2014; 6: 210–220.
Park S, Kim S, Park EM, Kim H, Kwon O, Chang C, et al. In vitro antimicrobial susceptibility of Mycobacterium abscessusin Korea. J Korean Med Sci 2008; 23: 49–52.
Kontos F, Mavromanolakis D, Zande M, Gitti Z. Isolation of Mycobacterium kumamotonensefrom a patient with pulmonary infection and latent tuberculosis. Indian J Med Microbiol 2016; 34: 241–244.
Griffith D, Aksamit T, Brown-Elliott B, Catanzaro A, Daley C, Gordin F, Holland S, Horsburgh R, Huitt G, Iademarco M, Iseman M, Olivier K, Ruoss S, von Reyn C, Wallace R, Winthrop K.An official ATS/ IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med 2007; 175: 367–416. 24. Arend SM, van Soolingen D, Ottenhoff T. Diagnosis and treatment of lung infection with nontuberculous mycobacteria. Curr Opin Pulm Med 2009; 15: 201–208.
Chetchotisakd P, Kiertiburanakul S, Mootsikapun P, Assanasen S, Chaiwarith R, Anunnatsiri S. Disseminated nontuberculous mycobacterial infection in patients who are not infected with HIV in Thailand. Clin Infect Dis Off Publ Infect Dis Soc Am 2007; 45: 421–427.
Scorzolini L, Mengoni F, Mastroianni CM, Baldan R, Cirillo DM, De Giusti M, Marinelli L, Cottarelli A, Fattorini L, Vullo V. Pseudo-outbreak of Mycobacterium gordonae in a teaching hospital: importance of strictly following decontamination procedures and emerging issues concerning sterilization. New Microbiol 2016; 39: 25–34.
Kapnadak S, Hisert K, Pottinger P, Limaye A, Aitken M. Infection control strategies that successfully controlled an outbreak of Mycobacterium abscessusat a cystic fibrosis center. Am J Infect Control 2016; 44: 154–159.
Ahmed I, Jabeen K, Hasan R. Identification of non-tuberculous mycobacteria isolated from clinical specimens at a tertiary care hospital: a cross-sectional study. BMC Infect Dis 2013; 13: 493.
Lim H, Park C, Park Y, Lee J, Lee S, Yang S, Yoo C, Kim Y, Han S, Yim J. Isolation of multiple nontuberculous mycobacteria species in the same patients. Int J Infect Dis 2011; 15: e795–e798.
Griffith D, Girard W, Wallace R. Clinical features of pulmonary disease caused by rapidly growing mycobacteria. An analysis of 154 patients. Am Rev Respir Dis 1993; 147: 1271–1278.
Tshikhudo P, Nnzeru R, Ntushelo K, Mudau F. Bacterial species identification getting easier. Afr J Biotechnol 2013; 12: 5975–5982.
Runyon, E. H.Anonymous mycobacteria in pulmonary disease. Med Clin of North Am 1959;43: 273-290.
Koh W, Kwon O, Lee K. Nontuberculous mycobacterial pulmonary diseases in immunocompetent patients. Korean J Radiol 2002; 3: 145–157.
Tortoli E, Bartoloni A, Bottger E, Emler S, Garzelli C, Magliano E, Mantella A, Rastogi N, Rindi L, Scarparo C, Urbano P. Burden of unidentifiable mycobacteria in a reference laboratory. J Clin Microbiol 2001; 39: 4058–4065.
Springer B, Stockman L, Teschner K, Roberts G, Böttger E. Two-laboratory collaborative study on identification of mycobacteria: molecular versus phenotypic methods. J Clin Microbiol 1996; 34: 296–303.
Chin’ombe N, Muzividzi B, Munemo E, Nziramasanga P. Molecular Identification of nontuberculous mycobacteria in humans in Zimbabwe using 16S ribosequencing. Open Microbiol J 2016; 10: 113–123.
Turenne C, Wallace R, Behr M. Mycobacterium aviumin the postgenomic era. Clin Microbiol Rev 2007; 20: 205–229.
Mijs W, de Haas P, Rossau R, Van der Laan T, Rigouts L, Portaels F, van Soolingen D. Molecular evidence to support a proposal to reserve the designation Mycobacterium aviumsubsp. aviumfor bird-type isolates and “M. aviumsubsp. hominissuis” for the human/porcine type of M. avium. Int J Syst Evol Microbiol 2002; 52: 1505–1518.
Turenne C, Semret M, Cousins D, Collins D, Behr M.Sequencing of hsp65distinguishes among subsets of the Mycobacterium aviumcomplex. J Clin Microbiol 2006; 44: 433–440.
Lee S, Kim B, Kim H, Won Y, Jeon C, Jeong J, Lee S, Lim J, Lee S, Kim C, Kook Y, Kim B. Mycobacterium paraintracellulare sp. nov., for the genotype INT-1 of Mycobacterium intracellulare. Int J Syst Evol Microbiol 2016; 66: 3132–3141.
Kobayashi T, Tsuyuguchi K, Yoshida S, Kurahara Y, Ikegami N, Naito M, Sonobe S, Maekura T, Tsuji T, Minomo S, Inoue Y, Suzuki K. Mycobacterium abscessussubsp. abscessuslung disease: drug susceptibility testing in sputum culture negative conversion. Int J Mycobacteriol 2018; 7: 69–75.
Caskey S, Moore J, Rendall J. In vitro activity of seven hospital biocides against Mycobacterium abscessus: Implications for patients with cystic fibrosis. Int J Mycobacteriol 2018; 7: 45–47.
Falkinham J. Nontuberculous mycobacteria from household plumbing of patients with nontuberculous mycobacteria disease. Emerg Infect Dis 2011; 17: 419–424.
Thomson R, Tolson C, Carter R, Coulter C, Huygens F, Hargreaves M. Isolation of nontuberculous mycobacteria (NTM) from household water and shower aerosols in patients with pulmonary disease caused by NTM. J Clin Microbiol 2013; 51: 3006– 3011.
Saiman L, Siegel J. Infection control in cystic fibrosis. Clin Microbiol Rev 2004; 17: 57–71.
Renna M, Schaffner C, Brown K, Shang S, Tamayo M, Hegyi K, Grimsey N, Cusens D, Coulter S, Cooper J, Bowden A, Newton S, Kampmann B, Helm J, Jones A, Haworth C, Basaraba R, DeGroote M, Ordway D, Rubinsztein D, Floto R. Azithromycin blocks autophagy and may predispose cystic fibrosis patients to mycobacterial infection. J Clin Invest 2011; 121: 3554–3563.
Bryant J, Grogono D, Greaves D, Foweraker J, Roddick I, Inns T, Reacher M, Haworth C, Curran M, Harris S, Peacock S, Parkhill J, Floto R.Whole-genome sequencing to identify transmission of Mycobacterium abscessusbetween patients with cystic fibrosis: a retrospective cohort study. Lancet Lond Engl 2013; 381: 1551–1560.
Tsukamura M. A group of mycobacteria from soil sources resembling nonphotochromogens (group 3). A description of Mycobacterium nonchromogenicum. Igaku To Seibutsugaku 1965; 71: 110–113.
Richmond L, Cummings M. An evaluation of methods of testing the virulence of acid-fast bacilli. Am Rev Tuberc 1950; 62: 632–637.
Kubica P, Silcox A, Kilburn J, Smithwick R, Beam R, Jones W, Stottmeier K. Differential identification of mycobacteria VI. Mycobacterium trivialeKubica sp. nov. Int J Syst Evol Microbiol 1970; 20: 161–174.
Tortoli E, Gitti Z, Klenk H-P, Lauria S, Mannino R, Mantegani P, Mariottini A, Neonakis I. Survey of 150 strains belonging to the Mycobacterium terraecomplex and description of Mycobacterium engbaekiisp. nov., Mycobacterium heraklionense sp. nov. and Mycobacterium longobardum sp. nov. Int J Syst Evol Microbiol 2013; 63: 401–411.
Smith D, Lindholm-Levy P, Huitt G, Heifets L, Cook J. Mycobacterium terrae: case reports, literature review, and in vitro antibiotic susceptibility testing. Clin Infect Dis Off Publ Infect Dis Soc Am 2000; 30: 444–453.
Díaz N, González F, Casado I, Galán L, Rojas M, Alado J. Lung infection by Mycobacterium terrae. Arch Bronconeumol 2001; 37: 96–98.
Sawai T, Inoue Y, Doi S, Izumikawa K, Ohno H, Yanagihara K, Higashiyama Y, Miyazaki Y, Hirakata Y, Tashiro T, Kohno S.A case of Mycobacterium nonchromogenicumpulmonary infection showing multiple nodular shadows in an immunocompetent patient. Diagn Microbiol Infect Dis 2006; 54: 311–314.
Kazda J, Cooney R, Monaghan M, Quinn P, Stackebrandt E, Dorsch M, Daffé M, Müller K, Cook B, Tarnok Z. Mycobacterium hiberniaesp. nov. Int J Syst Bacteriol 1993; 43: 352–357.
Masaki T, Ohkusu K, Hata H, Fujiwara N, Iihara H, Yamada-Noda M, Nhung P, Hayashi M, Asano Y, Kawamura Y, Ezaki T. Mycobacterium kumamotonensesp. nov. recovered from clinical specimen and the first isolation report of Mycobacterium arupense in Japan: Novel slowly growing, nonchromogenic clinical isolates related to Mycobacterium terraecomplex. Microbiol Immunol 2006; 50: 889–897.
Mun H, Park J, Kim H, Yu H, Park Y, Cha C, Kook Y, Kim B. Mycobacterium senuense sp. nov., a slowly growing, non-chromogenic species closely related to the Mycobacterium terraecomplex. Int J Syst Evol Microbiol 2008; 58: 641–646.
Lee H, Lee S, Lee I, Yu H, Park Y, Jeong J, Lee S, Kim S, Hyun J, Kim K, Kook Y, Kim B. Mycobacterium paraterraesp. nov. recovered from a clinical specimen: novel chromogenic slow growing mycobacteria related to Mycobacterium terraecomplex. Microbiol Immunol 2010; 54: 46–53.
Zhang Z, Sun Z, Wang Z, Wen Z, Sun Q, Zhu Z, Song Y, Zhao J, Wang H, Zhang S, Guo X. Complete genome sequence of a novel clinical isolate, the nontuberculous Mycobacterium strain JDM601. J Bacteriol 2011; 193: 4300–4301.
Tasler G, Hartley W. Foal abortion associated with Mycobacterium terraeinfection. Vet Pathol 1981; 18: 122–125. 61. Ngeow Y, Wong Y, Tan J, Hong K, Ng H, Ong B, Chan K. Identification of New Genomospecies in the Mycobacterium terrae complex. Plos One 2015; 10: e0120789. 1-16.
Brown-Elliott B, Wallace R. Clinical and taxonomic status of pathogenic nonpigmented or late-pigmenting rapidly growing mycobacteria. Clin Microbiol Rev 2002; 15: 716–746.
Schinsky M, Morey R, Steigerwalt A, Douglas M, Wilson R, Floyd M, Butler W, Daneshvar M, Brown-Elliott B, Wallace R Jr, McNeil M, Brenner D, Brown J.Taxonomic variation in the Mycobacterium fortuitum third biovariant complex: description of Mycobacterium boenickeisp. nov., Mycobacterium houstonensesp. nov., Mycobacterium neworleansensesp. nov. and Mycobacterium brisbanensesp. nov. and recognition of Mycobacterium porcinum from human clinical isolates. Int J Syst Evol Microbiol 2004; 54: 1653–1667.
Wallace R, Brown-Elliott B, Hall L, Roberts G, Wilson R, Mann L, Crist C, Chiu S, Dunlap R, Garcia M, Bagwell J, Jost K Jr.. Clinical and laboratory features of Mycobacterium mageritense. J Clin Microbiol 2002; 40: 2930–2935.
Han X, Dé I, Jacobson K. Rapidly growing mycobacteria: clinical and microbiologic studies of 115 Cases. Am J Clin Pathol 2007; 128: 612–621.
Lamy B, Marchandin H, Hamitouche K, Laurent F. Mycobacterium setensesp. nov., a Mycobacterium fortuitum-group organism isolated from a patient with soft tissue infection and osteitis. Int J Syst Evol Microbiol 2008; 58: 486–490.
Ucko M, Colorni A, Kvitt H, Diamant A, Zlotkin A, Knibb W. Strain Variation in Mycobacterium marinumfish isolates. Appl Environ Microbiol 2002; 68: 5281–5287.
Hess C, Wolock B, Murphy M. Mycobacterium marinuminfections of the upper extremity. Plast Reconstr Surg 2005; 115: 55e-59e.
Stinear T, Mve-Obiang A, Small P, Frigui W, Pryor M, Brosch R, Jenkin G, Johnson P, Davies J, Lee R, Adusumilli S, Garnier T, Haydock S, Leadlay P, Cole S.Giant plasmid-encoded polyketide synthases produce the macrolide toxin of Mycobacterium ulcerans. Proc Natl Acad Sci U S A 2004; 101: 1345–1349.
Stinear T, Seemann T, Pidot S, Frigui W, Reysset G, Garnier T, Meurice G, Simon D, Bouchier C, Ma L, Tichit M, Porter J, Ryan J, Johnson P, Davies J, Jenkin G, Small P, Jones L, Tekaia F, Laval F, Daffé M, Parkhill J, Cole S.Reductive evolution and niche adaptation inferred from the genome of Mycobacterium ulcerans, the causative agent of buruli ulcer. Genome Res 2007; 17: 192–200.
Slany M, Makovcova J, Jezek P, Bodnarova M, Pavlik I. Relative prevalence of Mycobacterium marinumin fish collected from aquaria and natural freshwaters in central Europe. J Fish Dis 2014; 37: 527–533.
Trott K, Stacy B, Lifland B, Diggs H, Harland R, Khokha M, Grammer T, Parker J. Characterization of a Mycobacterium ulcerans-like infection in a colony of african tropical clawed frogs (Xenopus tropicalis). Comp Med 2004; 54: 309–317.
Mve-Obiang A, Lee R, Umstot E, Trott K, Grammer T, Parker J, Ranger B, Grainger R, Mahrous E, Small P. A newly discovered mycobacterial pathogen isolated from laboratory colonies of Xenopusspecies with lethal infections produces a novel form of mycolactone, the Mycobacterium ulcerans macrolide toxin. Infect Immun 2005; 73: 3307–3312.
Tobias N, Doig K, Medema M, Chen H, Haring V, Moore R, Seemann T, Stinear T.Complete genome sequence of the frog pathogen Mycobacterium ulceransEcovar Liflandii. J Bacteriol 2013; 195: 556–564.
Tortoli E, Böttger E, Fabio A, Falsen E, Gitti Z, Grottola A, Klenk H, Mannino R, Mariottini A, Messinò M, Pecorari M, Rumpianesi F. Mycobacterium europaeum sp. nov., a scotochromogenic species related to the Mycobacterium simiaecomplex. Int J Syst Evol Microbiol 2011; 61: 1606–1611.
Bouam A, Heidarieh P, Shahraki A, Pourahmad F, Mirsaeidi M, Hashemzadeh M, Baptiste E, Armstrong N, Levasseur A, Robert C, Drancourt M. Mycobacterium ahvazicumsp. nov., the nineteenth species of theMycobacterium simiae complex. Sci Rep 2018; 8: 4138- 4149. 77. Adékambi T, Drancourt M. Dissection of phylogenetic relationships among 19 rapidly growing Mycobacteriumspecies by 16S rRNA, hsp65, sodA, recAand rpoBgene sequencing. Int J Syst Evol Microbiol 2004; 54: 2095–2105.
Adékambi T, Berger P, Raoult D, Drancourt M. rpoBgene sequence-based characterization of emerging non-tuberculous mycobacteria with descriptions of Mycobacterium bolletiisp. nov., Mycobacterium phocaicumsp. nov. and Mycobacterium aubagnensesp. nov. Int J Syst Evol Microbiol 2006; 56: 133–143.
Adékambi T. Mycobacterium mucogenicum group infections: a review. Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis 2009; 15: 911–918.
Lamrabet O, Medie F, Drancourt M. Acanthamoeba polyphaga-enhanced growth of Mycobacterium smegmatis. Plos One 2012; 7: e29833. 1-8.
Eid A, Berbari E, Sia I, Wengenack N, Osmon D, Razonable R. Prosthetic joint infection due to rapidly growing mycobacteria: report of 8 cases and review of the literature. Clin Infect Dis Off Publ Infect Dis Soc Am 2007; 45: 687–694.
Chen Y, Jou R, Huang W, Huang S, Liu K, Lay C, Chang S, Tseng C, Lai C, Su Y. Bacteremia caused by Mycobacterium wolinskyi. Emerg Infect Dis 2008; 14: 1818– 1819.
Gupta R, Lo B, Son J. Phylogenomics and comparative genomic studies robustly support division of the genus Mycobacteriuminto an emended genus Mycobacteriumand four novel genera. Front Microbiol 2018; 9: 67-78.
Purcaro G, Tranchida P, Dugo P, La Camera E, Bisignano G, Conte L, Mondello L. Characterization of bacterial lipid profiles by using rapid sample preparation and fast comprehensive two-dimensional gas chromatography in combination with mass spectrometry. J Sep Sci 2010; 33: 2334–2340.
Butler W, Guthertz L. Mycolic acid analysis by high-performance liquid chromatography for identification of Mycobacterium Species. Clin Microbiol Rev 2001; 14: 704– 726.
Jost K, Dunbar D, Barth S, Headley V, Elliott L. Identification of Mycobacterium tuberculosisand M. aviumcomplex directly from smear-positive sputum specimens and BACTEC 12B cultures by high-performance liquid chromatography with fluorescence detection and computer-driven pattern recognition models. J Clin Microbiol 1995; 33: 1270–1277.
Butler W, Jost K, Kilburn J. Identification of mycobacteria by high-performance liquid chromatography. J Clin Microbiol 1991; 29: 2468–2472.
Glickman S, Kilburn J, Butler W, Ramos L. Rapid identification of mycolic acid patterns of mycobacteria by high-performance liquid chromatography using pattern recognition software and a Mycobacterium library. J Clin Microbiol 1994; 32: 740–745.
Cloud J, Meyer J, Pounder J, Jost K, Sweeney A, Carroll K, Woods G. Mycobacterium arupensesp. nov., a non-chromogenic bacterium isolated from clinical specimens. Int J Syst Evol Microbiol 2006; 56: 1413–1418.
Cooksey R, Jhung M, Yakrus M, Butler W, Adékambi T, Morlock G, Williams M, Shams A, Jensen B, Morey R, Charles N, Toney S, Jost K Jr, Dunbar D, Bennett V, Kuan M, Srinivasan A.Multiphasic approach reveals genetic diversity of environmental and patient isolates of Mycobacterium mucogenicumand Mycobacterium phocaicum associated with an outbreak of bacteremias at a Texas hospital. Appl Environ Microbiol 2008; 74: 2480–2487.
Lane D, Pace B, Olsen G, Stahl D, Sogin M, Pace N. Rapid determination of 16S ribosomal RNA sequences for phylogenetic analyses. Proc Natl Acad Sci U S A 1985; 82: 6955–6959.
Woese C, Stackebrandt E, Macke T, Fox G. A phylogenetic definition of the major eubacterial taxa. Syst Appl Microbiol 1985; 6: 143–151.
Woese C. Bacterial evolution. Microbiol Rev 1987; 51: 221–271.
Chakravorty S, Helb D, Burday M, Connell N, Alland D. A detailed analysis of 16S ribosomal RNA gene segments for the diagnosis of pathogenic bacteria. J Microbiol Methods 2007; 69: 330–339.
Vetrovský T, Baldrian P. The variability of the 16S rRNA gene in bacterial genomes and its consequences for bacterial community analyses. Plos One 2013; 8: e57923. 1-10.
Dahllöf I, Baillie H, Kjelleberg S. rpoBbased microbial community analysis avoids limitations inherent in 16S rRNA gene intraspecies heterogeneity. Appl Environ Microbiol 2000; 66: 3376–3380.
Case R, Boucher Y, Dahllöf I, Holmström C, Doolittle W, Kjelleberg S. Use of 16S rRNA and rpoBgenes as molecular markers for microbial ecology studies. Appl Environ Microbiol 2007; 73: 278–288.
Candela M, Vitali B, Matteuzzi D, Brigidi P. Evaluation of the rrnoperon copy number in Bifidobacteriumusing real-time PCR. Lett Appl Microbiol 2004; 38: 229-232.
Lee C, Sieo C, Abdullah N, Ho Y. Estimation of 16S rRNA gene copy number in several probiotic Lactobacillusstrains isolated from the gastrointestinal tract of chicken. FEMS Microbiol Lett 2008; 287: 136-141.
Fox G, Wisotzkey J, Jurtshuk P. How close is close: 16S rRNA sequence identity may not be sufficient to guarantee species identity. Int J Syst Bacteriol 1992; 42: 166–170.
Stackebrandt E, Goebel B. Taxonomic Note: A place for DNA-DNA reassociation and 16S rRNA sequence analysis in the present species definition in bacteriology. Int J Syst Evol Microbiol 1994; 44: 846–849.
Park H, Jang H, Kim C, Chung B, Chang C, Park S, Song S. Detection and identification of mycobacteria by amplification of the internal transcribed spacer regions with genus- and species-specific PCR primers. J Clin Microbiol 2000; 38: 4080–4085.
Gopinath K, Singh S. Multiplex PCR assay for simultaneous detection and differentiation of Mycobacterium tuberculosis, Mycobacterium aviumcomplexes and other mycobacterial species directly from clinical specimens. J Appl Microbiol 2009; 107: 425–435.
Ngan G, Ng L, Jureen R, Lin R, Teo J. Development of multiplex PCR assays based on the 16S-23S rRNA internal transcribed spacer for the detection of clinically relevant nontuberculous mycobacteria. Lett Appl Microbiol 2011; 52: 546–554.
Mwikuma G, Kwenda G, Hang’ombe B, Simulundu E, Kaile T, Nzala S, Siziya S, Suzuki Y. Molecular identification of nontuberculous mycobacteria isolated from clinical specimens in Zambia. Ann Clin Microbiol Antimicrob 2015; 14: 1-5.
Park J, Shim T, Lee S, Lee H, Lee I, Kim K, Kook Y, Kim B. Molecular characterization of Mycobacterium intracellulare-related strains based on the sequence analysis of hsp65, internal transcribed spacer and 16S rRNA genes. J Med Microbiol 2010; 59: 1037–1043.
Stout J, Hopkins G, McDonald J, Quinn A, Hamilton C, Reller L, Frothingham R. Association between 16S-23S internal transcribed spacer sequence groups of Mycobacterium aviumcomplex and pulmonary disease. J Clin Microbiol 2008; 46: 2790– 2793.
Subedi S, Kong F, Jelfs P, Gray T, Xiao M, Sintchenko V, Chen S. 16S-23S Internal transcribed spacer region PCR and sequencer-based capillary gel electrophoresis has potential as an alternative to high performance liquid chromatography for identification of slowly growing nontuberculous mycobacteria. Plos One 2016; 11: e0164138. 1-15.
Tortoli E. Impact of genotypic studies on mycobacterial taxonomy: the new mycobacteria of the 1990s. Clin Microbiol Rev 2003; 16: 319–354.
De Bruyne K, Slabbinck B, Waegeman W, Vauterin P, De Baets B, Vandamme P.Bacterial species identification from MALDITOF mass spectra through data analysis and machine learning. Syst Appl Microbiol 2011; 34: 20–29.
Hettick J, Kashon M, Slaven J, Ma Y, Simpson J, Siegel P, Mazurek G, Weissman D. Discrimination of intact mycobacteria at the strain level: a combined MALDI-TOF MS and biostatistical analysis. Proteomics 2006; 6: 6416–6425.
Mediavilla-Gradolph M, De Toro-Peinado I, Bermúdez-Ruiz M, García-Martínez M de los Á, Ortega-Torres M, Montiel QuezelGuerraz N, Palop-Borrás B. Use of MALDITOF MS for Iidentification of nontuberculous Mycobacteriumspecies isolated from clinical specimens. BioMed Res Int 2015. 2015; 854078. 1-6.
Saleeb P, Drake S, Murray P, Zelazny A. Identification of mycobacteria in solid culture media by matrix-assisted laser desorption ionization-time of flight mass spectrometry. J Clin Microbiol 2011; 49: 1790–1794.
Cao Y, Wang L, Ma P, Fan W, Gu B, Ju S. Accuracy of matrix-assisted laser desorption ionization-time of flight mass spectrometry for identification of mycobacteria: a systematic review and meta-analysis. Sci Rep 2018; 8: 4131-4139.
Plikaytis B, Plikaytis B, Yakrus M, Butler W, Woodley C, Silcox V, et al. Differentiation of slowly growing Mycobacteriumspecies, including Mycobacterium tuberculosis, by gene amplification and restriction fragment length polymorphism analysis. J Clin Microbiol 1992; 30: 1815–1822.
Telenti A, Marchesi F, Balz M, Bally F, Böttger E, Bodmer T. Rapid identification of mycobacteria to the species level by polymerase chain reaction and restriction enzyme analysis. J Clin Microbiol 1993; 31: 175–178.
Kirschner P, Böttger E. Microheterogeneity within rRNA of Mycobacterium gordonae. J Clin Microbiol 1992; 30: 1049–1050.
Taylor T, Patterson C, Hale Y, Safranek W. Routine use of PCR-restriction fragment length polymorphism analysis for identification of mycobacteria growing in liquid media. J Clin Microbiol 1997; 35: 79–85.
Devallois A, Goh K, Rastogi N. Rapid identification of mycobacteria to species level by PCR-restriction fragment length polymorphism analysis of the hsp65gene and proposition of an algorithm to differentiate 34 mycobacterial species. J Clin Microbiol 1997; 35: 2969–2973.
Brunello F, Ligozzi M, Cristelli E, Bonora S, Tortoli E, Fontana R. Identification of 54 mycobacterial species by PCR-restriction fragment length polymorphism analysis of the hsp65gene. J Clin Microbiol 2001; 39: 2799–2806.
Alcaide F, Richter I, Bernasconi C, Springer B, Hagenau C, Schulze-Röbbecke R, Tortoli E, Martín R, Böttger E, Telenti A. Heterogeneity and clonality among isolates of Mycobacterium kansasii: implications for epidemiological and pathogenicity studies. J Clin Microbiol 1997; 35: 1959–1964.
Kim H, Kim S, Shim T, Kim M, Bai G, Park Y, Lee S, Cha C, Kook Y, Kim B. PCR restriction fragment length polymorphism analysis (PRA)-algorithm targeting 644 bp Heat Shock Protein 65 (hsp65) gene for differentiation of Mycobacteriumspp. J Microbiol Methods 2005; 62: 199–209.
Ong C, Ngeow Y, Yap S, Tay S. Evaluation of PCR-RFLP analysis targeting hsp65and rpoBgenes for the typing of mycobacterial isolates in Malaysia. J Med Microbiol 2010; 59: 1311–1316.
Gingeras T, Ghandour G, Wang E, Berno A, Small P, Drobniewski F, Alland D, Desmond E, Holodniy M, Drenkow J. Simultaneous genotyping and species identification using hybridization pattern recognition analysis of generic MycobacteriumDNA arrays. Genome Res 1998; 8: 435–448.
Lee H, Bang H, Bai G, Cho S. Novel polymorphic region of the rpoBgene containing Mycobacteriumspecies-specific sequences and its use in identification of mycobacteria. J Clin Microbiol 2003; 41: 2213–2218.
Musser J. Antimicrobial agent resistance in mycobacteria: Molecular genetic insights. Clin Microbiol Rev 1995; 8. 496- 514.
Boor K, Duncan M, Price C. Genetic and transcriptional organization of the region encoding the beta subunit of Bacillus subtilisRNA polymerase. J Biol Chem 1995; 270: 20329–20336.
Kim B, Lee S, Lyu M, Kim S, Bai G, Chae G, Kim E, Cha C, Kook Y. Identification of mycobacterial species by comparative sequence analysis of the RNA polymerase gene (rpoB). J Clin Microbiol 1999; 37: 1714–1720.
Troesch A, Nguyen H, Miyada C, Desvarenne S, Gingeras T, Kaplan P, Cros P, Mabilat C. Mycobacteriumspecies identification and rifampin resistance testing with high-density DNA probe arrays. J Clin Microbiol 1999; 37: 49–55.
Lee H, Park H, Cho S, Bai G, Kim S. Species identification of mycobacteria by PCRrestriction fragment length polymorphism of the rpoBgene. J Clin Microbiol 2000; 38: 2966–2971.
Kim B, Lee K, Park B, Kim S, Bai G, Kim S, Kook Y. Differentiation of mycobacterial species by PCR-restriction analysis of DNA (342 base pairs) of the RNA polymerase gene (rpoB). J Clin Microbiol 2001; 39: 2102–2109. 132. de Zwaan R, van Ingen J, van Soolingen D. Utility of rpoB gene sequencing for identification of nontuberculous mycobacteria in the Netherlands. J Clin Microbiol 2014; 52: 2544–2551.
Simmon K, Pounder J, Greene J, Walsh F, Anderson C, Cohen S, Petti C. Identification of an emerging pathogen,Mycobacterium massiliense, by rpoB sequencing of clinical isolates collected in the United States. J Clin Microbiol 2007; 45: 1978–1980.
Ben Salah I, Adékambi T, Raoult D, Drancourt M. rpoB sequence-based identification of Mycobacterium aviumcomplex species. Microbiol Read Engl 2008; 154: 3715–3723.
Somoskovi A, Song Q, Mester J, Tanner C, Hale Y, Parsons L, Salfinger M. Use of molecular methods to identify the Mycobacterium tuberculosiscomplex (MTBC) and other mycobacterial species and to detect rifampin resistance in MTBC isolates following growth detection with the BACTEC MGIT 960 system. J Clin Microbiol 2003; 41: 2822–2826.
Lee A, Jelfs P, Sintchenko V, Gilbert G. Identification of non-tuberculous mycobacteria: utility of the GenoType MycobacteriumCM/AS assay compared with HPLC and 16S rRNA gene sequencing. J Med Microbiol 2009; 58: 900–904.
García-Agudo L, Jesús I, Rodríguez-Iglesias M, García-Martos P. Evaluation of INNO-LiPA mycobacteria v2 assay for identification of rapidly growing mycobacteria. Braz J Microbiol Publ Braz Soc Microbiol 2011; 42: 1220–1226.
Sarkola A, Mäkinen J, Marjamäki M, Marttila H, Viljanen M, Soini H. Prospective evaluation of the GenoType assay for routine identification of mycobacteria. Eur J Clin Microbiol Infect Dis Off Publ Eur Soc Clin Microbiol 2004; 23: 642–645.
Ruiz P, Gutierrez J, Zerolo F, Casal M. GenoType Mycobacteriumassay for identification of mycobacterial species isolated from human clinical samples by using liquid medium. J Clin Microbiol 2002; 40: 3076–3078.
Richter E, Rüsch-Gerdes S, Hillemann D. Evaluation of the GenoType Mycobacteriumassay for identification of mycobacterial species from cultures. J Clin Microbiol 2006; 44: 1769–1775.
Turenne C, Collins D, Alexander D, Behr M. Mycobacterium aviumsubsp. paratuberculosisand M. aviumsubsp. aviumare independently evolved pathogenic clones of a much broader group of M. aviumorganisms. J Bacteriol 2008; 190: 2479–2487.
Devulder G, Pérouse de Montclos M, Flandrois J. A multigene approach to phylogenetic analysis using the genus Mycobacteriumas a model. Int J Syst Evol Microbiol 2005; 55: 293–302.
Macheras E, Roux A, Ripoll F, SivadonTardy V, Gutierrez C, Gaillard J, Heym B. Inaccuracy of single-target sequencing for discriminating species of the Mycobacterium abscessusgroup. J Clin Microbiol 2009; 47: 2596–2600.
Stackebrandt E, Frederiksen W, Garrity G, Grimont P, Kämpfer P, Maiden M, Nesme X, Rosselló-Mora R, Swings J, Trüper H, Vauterin L, Ward A, Whitman W.Report of the ad hoc committee for the re-evaluation of the species definition in bacteriology. Int J Syst Evol Microbiol 2002; 52: 1043–1047.
Rosselló-Mora R, Amann R. The species concept for prokaryotes. FEMS Microbiol Rev 2001; 25: 39–67.
Mignard S, Flandrois J. A seven-gene, multilocus, genus-wide approach to the phylogeny of mycobacteria using supertrees. Int J Syst Evol Microbiol 2008; 58: 1432–1441.
Macheras E, Roux A, Bastian S, Leão S, Palaci M, Sivadon-Tardy V, Gutierrez C, Richter E, Rüsch-Gerdes S, Pfyffer G, Bodmer T, Cambau E, Gaillard J, Heym B. Multilocus sequence analysis and rpoB sequencing of Mycobacterium abscessus (sensu lato) strains. J Clin Microbiol 2011; 49: 491–499.
Leao S, Tortoli E, Viana-Niero C, Ueki S, Lima K, Lopes M, Yubero J, Menendez M, Garcia M. Characterization of mycobacteria from a major brazilian outbreak suggests that revision of the taxonomic status of members of the Mycobacterium chelonae-M. abscessus group is needed. J Clin Microbiol 2009; 47: 2691–2698.
Köser C, Ellington M, Cartwright E, Gillespie S, Brown N, Farrington M, Holden M, Dougan G, Bentley S, Parkhill J, Peacock S. Routine use of microbial whole genome sequencing in diagnostic and public health microbiology. Plos Pathog 2012; 8: e1002824. 1-9.
Loman N, Pallen M. XDR-TB genome sequencing: a glimpse of the microbiology of the future. Future Microbiol 2008; 3: 111–113.
Tettelin H, Davidson R, Agrawal S, Aitken M, Shallom S, Hasan N, Strong M, de Moura V, De Groote M, Duarte R, Hine E, Parankush S, Su Q, Daugherty S, Fraser C, Brown-Elliott B, Wallace R Jr, Holland S, Sampaio E, Olivier K, Jackson M, Zelazny A. High-level relatedness among Mycobacterium abscessussubsp. massiliense strains from widely separated outbreaks. Emerg Infect Dis 2014; 20: 364–371.
Wee W, Tan T, Jakubovics N, Choo S. Whole-genome sequencing and comparative analysis of Mycobacterium brisbanense reveals a possible soil origin and capability in fertiliser synthesis. Plos One 2016; 11: e0152682. 1-15.
Köser C, Holden M, Ellington M, Cartwright E, Brown N, Ogilvy-Stuart A, Hsu L, Chewapreecha C, Croucher N, Harris S, Sanders M, Enright M, Dougan G, Bentley S, Parkhill J, Fraser L, Betley J, SchulzTrieglaff O, Smith G, Peacock S.Rapid whole-genome sequencing for investigation of a neonatal MRSA outbreak. N Engl J Med 2012; 366: 2267–2275.
Pallen M, Loman N, Penn C.High-throughput sequencing and clinical microbiology: progress, opportunities and challenges. Curr Opin Microbiol 2010; 13: 625–631.
Underwood A, Green J. Call for a quality standard for sequence-based assays in clinical microbiology: necessity for quality assessment of sequences used in microbial identification and typing. J Clin Microbiol 2011; 49: 23–26.
Tran A, Alby K, Kerr A, Jones M, Gilligan P. Cost savings realized by implementation of routine microbiological identification by matrix-assisted laser desorption ionizationtime of flight mass spectrometry. J Clin Microbiol 2015; 53: 2473–2479.
Schlatter R, Matte U, Polanczyk C, Koehler-Santos P, Ashton-Prolla P. Costs of genetic testing: supporting brazilian public policies for the incorporating of molecular diagnostic technologies. Genet Mol Biol 2015; 38: 332–337.
Mondragón-Barreto M, Vázquez-Chacón C, Barrón-Rivero C, Acosta-Blanco P, Jost K, Balandrano S, Olivera-Díaz H. Comparison among three methods for mycobacteria identification. Salud Publica Mex 2000; 42: 484–489.
Kellogg J, Bankert D, Withers G, Sweimler W, Kiehn T, Pfyffer G. Application of the Sherlock mycobacteria identification system using high-performance liquid chromatography in a clinical laboratory. J Clin Microbiol 2001; 39: 964–970.
Schwarze K, Buchanan J, Taylor J, Wordsworth S. Are whole-exome and whole-genome sequencing approaches cost-effective? A systematic review of the literature. Genet Med Off J Am Coll Med Genet 2018; 1-9.
van Ingen J. Microbiological diagnosis of nontuberculous mycobacterial pulmonary disease. In: Huitt G, Dayley C (Ed). Nontuberculous mycobacteria, an issue of clinics in chest medicine. Philadelphia- Pennsylvania. Elsevier 2015; P 47-48.
Pankhurst L, Del Ojo Elias C, Votintseva A, Walker T, Cole K, Davies J, Fermont J, Gascoyne-Binzi D, Kohl T, Kong C, Lemaitre N, Niemann S, Paul J, Rogers T, Roycroft E, Smith E, Supply P, Tang P, Wilcox M, Wordsworth S, Wyllie D, Xu L, Crook D.Rapid, comprehensive, and affordable mycobacterial diagnosis with whole-genome sequencing: a prospective study. Lancet Respir Med 2016; 4: 49–58.